Many patients with sickle cell disease (SCD) require chronic transfusions and are at risk for life-threatening delayed hemolytic transfusion reactions (DHTRs). The diagnosis of DHTR is often difficult because antibodies against the transfused RBCs are often undetectable and symptoms can mimic vaso-occlusive events. Presently, there are no existing guidelines or evidence-based studies to guide the prevention, diagnosis, and treatment of DHTR. In order to provide some guidance, doctors at a French hospital shared their expertise and assessment criteria to diagnose and treat DHTRs in SCD patients. They have devised a DHTR risk score for patients receiving episodic transfusions based on three criteria—history of RBC alloimmunization, number of previous transfusions, and previous DHTRs. They recommend transfusing matching Rh and K RBCs in SCD patients with a low risk of DHTR and extending matching to Fy, Jk and Ss in higher risk patients. If DHTR is suspected, they have devised a nomogram based on post-transfusion total Hb and HbA% to help diagnosis DHTR. They also recommend prophylactic rituximab for high risk patients or DHTR patients requiring transfusions. Intravenous immunoglobulin, erythropoietin, high-dose steroids, eculizumab, and plasma exchange may also be tailored for individual DHTR treatment. However, additional studies for the prevention, diagnosis, treatment of DHTR are critically needed.
Reference:

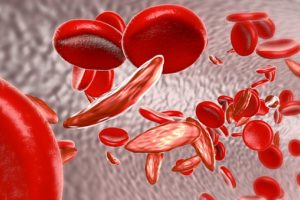
The issue with treating SCD, rests purely on the chronic transfusions. Due to multiple transfusions, the patient is exposed to multiple antibodies which likely go under detected due to the state of the patient plus the list of medication that has been taken. Should a more synthetic/artificial blood product be used to treat these patients, it would lessen the exposure to foreign bodies and also the process would be less life-threatening for the patient.