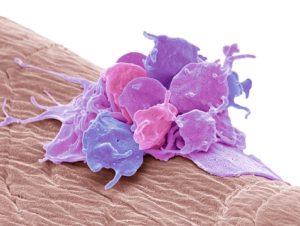
Wound healing is a multistep process involving many different types of cells, growth factors, and cytokines. Platelets are key to initiate wound healing; once activated at the wound site, platelets release chemical signals to activate fibrin-platelet clots and draw white blood cells to the wound site to clear out damaged, dead, or pathogenic cells. Growth factors and cytokines released by platelets also promote tissue repair, influence angiogenesis, and inflammation at the wound site. However, little is known about the effectiveness of using autologous platelet-rich plasma (PRP) as a therapeutic option to improve wound healing. Researchers from the Netherlands generated platelet pools approximately 3- to 4-fold more concentrated (compared to physiological levels). Platelet concentrates were resuspended in plasma (PC-plasma) or platelet additive solution (PC-PAS) and the effects of PC-plasma, PC-PAS, and plasma for in vitro wound healing assays were measured. PC-plasma significantly increased fibroblast proliferation and migration as compared to PC-PAS or plasma. Furthermore, PC-plasma and plasma alone both stimulated the angiogenic sprouting of endothelial cells significantly more than PC-PAS, and PC-plasma was superior in stimulating chemotaxis of white blood cells compared to PC-PAS or plasma. Further research should explore the effectiveness and dosage regime of PC-plasma on in vivo wound healing.
Reference: