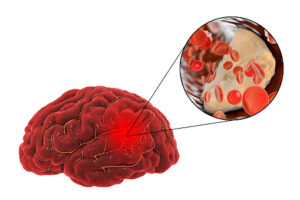
Historically, standard practice has been to provide ABO-compatible platelets when possible. However, since hemolysis is rare after single platelet transfusions and because of limited platelet availability, a significant proportion of platelet transfusions are ABO incompatible. Nevertheless, data from the Platelet Transfusion in Spontaneous Intracerebral Hemorrhage on Antiplatelet Agents (PATCH) trial in 2016 found that platelet transfusions given to reverse antiplatelet medications may actually increase mortality and disability in patients with intracerebral hemorrhage (ICH). In order to investigate the role that incompatible platelets may play in worsening patient prognosis after platelet transfusions, researchers at Columbia University identified 125 patients with ICH receiving platelet transfusions, of which 38% (47/125) were ABO incompatible. ABO incompatible platelet transfusions were associated with lower platelet recovery (p=0.01) and increased odds of mortality (p=0.05). Further studies are needed to confirm and understand the mechanism behind worse outcomes after incompatible platelet transfusions in select patient populations.
References:
- Magid-Bernstein J, Beaman CB, Carvalho-Poyraz F, Boehme A, et al. Impacts of ABO-incompatible platelet transfusions on platelet recovery and outcomes after intracerebral hemorrhage. Blood 2021; 137(19); 2699-2703.
- Devine DV. Rethinking platelet transfusion practices. Blood 2021; 137(19); 2576-2577.