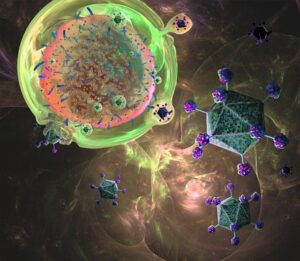
Chimeric antigen receptor (CAR) T-cell therapy is a promising therapy used to treat hematological cancers by targeting a specific antigen. Notably, CD19 CAR T-cell therapy has a 90% complete response rate in children and adults with acute lymphoblastic leukemia (ALL), but it is unclear why about 10% of patients do not respond to treatment. In order to gain insights, researchers at the U.S. National Institute of Health and the National Cancer Institute retrospectively searched three public U.S. and European databases for CAR T-cell therapy clinical outcomes with gene expression profile data for both pediatric and adult ALL patients. Two data sets with a total of 31 patients were identified; 22 of the 31 patients achieved a compete response with CD19 CAR T-cell therapy. However, nine patients showed no response to treatment. By examining the transcriptomic profile of the recipient bone marrow prior to lymphodepleting preconditioning using several methods (principal component analysis, fold change, gene ontology, and gene set analyses), a 14-gene signature was identified as a predictor for clinical outcome. Patients with a complete response to CAR T-cell therapy had preconditioning transcriptomic profiles that enhanced T-cell activation and differentiation. Patients who did not respond to CAR T-cell therapy had profiles with higher activity in cell cycle checkpoints. The transcriptomic profile of the bone marrow as well as tumor characteristics, disease severity and molecular phenotype, and CD19 CAR T-cell expansion all seem to play a role in the efficacy of CAR T-cell therapy for ALL, but further investigation is needed.
Reference: