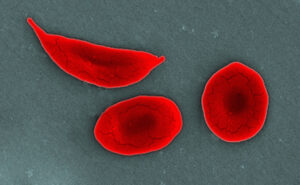
Unlike patients with intravascular hemolysis without sickle cell disease (SCD) or those with β-thalassemia, patients with SCD have elevated baseline levels of proinflammatory cytokines which increase during vaso-occlusive crises (VOC). Monocytes are responsible for the increased production of these cytokines, but the mechanisms behind the activation of monocytes in patients with SCD have been elusive. Allali et al. have shown that cell-free hemoglobin S (HbS), and not hemoglobin A or heme, increases proinflammatory cytokines (e.g., TNF-α, IL-1β, and IL-6) in cultured human monocytes and in mice by directly interacting with the Toll-like receptor 4 (TLR4)/myeloid differentiation factor 2 (MD-2) complex. Activation of monocytes by HbS was abrogated by adding a TLR4 inhibitor or when using monocytes lacking TLR4. The authors hypothesized that the single replacement of hydrophilic glutamic acid at position 6 in the β-chain of hemoglobin with hydrophobic valine in sickle cell HbS may allow HbS to bind the hydrophobic binding pocket within MD-2, thus promoting TLR4-mediated monocyte activation and cytokine production. Indeed, the authors show that HbS has a strong affinity for the TLR4/MD-2 complex. Although multiple mechanisms may lead to proinflammatory cytokine production in patients with SCD, disruption of the HbS/TLR4 interaction may lead to novel treatments for SCD.
References:
- Allali S, Rignault-Bricard R, de Montalembert M, Taylor M, et al. HbS promotes TLR4-mediated monocyte activation and proinflammatory cytokine production in sickle cell disease. Blood 2022; 140(18); 1972-1982.
- Gibb DR and KE Hudson. Sickle cell inflammation: is HbS the answer? Blood 2022; 140(18); 1921-1023.