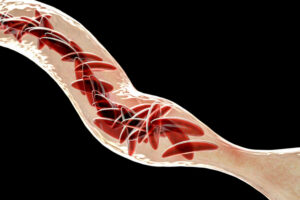
RBC transfusions are critical for many patients with sickle cell disease. Patients are at risk, however, of developing alloantibodies, which complicates future RBC transfusions. To understand the chronology of alloantibody formation and identify characteristics of high- and low-responders, researchers in France retrospectively followed 6496 RH-K matched transfused patients with sickle cell disease from 2008 to 2018. Each patient received between one and 1372 units of RBCs over the 11-year study period, and 30% (1742/6020) became alloimmunized. By the 20th RBC unit transfusion, 75% of patients who would become alloimmunized (excluding warm autoantibodies) had developed antibodies to at least one antigen. The mean age of first alloimmunization was 12 years; women of childbearing age formed antibodies earlier than males (p=0.005), but there was no difference between children or older adults. Almost half (48%) of patients made antibodies to multiple antigens and the most frequent antibodies were warm autoantibodies, antibodies of undetermined specificity, and anti-C. Patients who developed warm autoantibodies first were less likely to become alloimmunized to other antigens than those who made antibodies to high-frequency antigens or antigens of the extended phenotype (e.g. RH-K, FY, JK, Ss). Further research is needed to determine factors affecting alloimmunization for patients who are chronically transfused.
Reference: