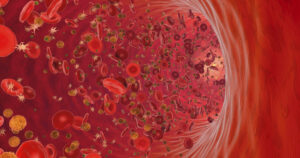
Red blood cells (RBCs) deliver oxygen to tissues and also contribute to hemostasis and thrombosis through platelet interactions that promote clot formation. In addition, RBC release adenosine 5′-diphosphate (ADP) and extracellular vesicles, which promote procoagulant conditions. It has also been observed that prolonged bleeding times can be reduced in anemic patients with RBC transfusions, but the physiology was unknown. To gain a better understanding of the effects of RBCs on hemostasis, researchers reconstituted human blood at varying hematocrits and perfused it over immobilized collagen in a microfluidic chamber to mimic arterial wall sheer stress after vascular injury. Increasing hematocrit increased platelet thrombus formation under flow conditions, but RBC membrane integrity was necessary for RBCs to promote platelet aggregation. Mice with pancytopenia induced by irradiation formed small platelet-poor clots at vascular injury sites, but clot size increased 3- to 5-fold when mice were transfused with RBCs suggesting that RBCs improve hemostasis even in the near absence of platelets. Further, results suggest that high sheer stress cause RBCs to release ADP and activate platelets and clot formation in patients with left ventricular assist devices. Additional studies are needed to better understand the role of RBCs in hemostasis.
References:
- Cheryl L. Maier, Wilbur A. Lam; Red blood cells: more than bags of hemoglobin. Blood 2024; 144 (14): 1467–1469
- Debbie Jiang, Katie L. Houck, Lydia Murdiyarso, Harrison Higgins, Nicole Rhoads, Sophia K. Romero, Rosemary Kozar, Angelo Nascimbene, Terry B. Gernsheimer, Zyrina Alura C. Sanchez, Anand K. Ramasubramanian, Reheman Adili, Jing-fei Dong; RBCs regulate platelet function and hemostasis under shear conditions through biophysical and biochemical means. Blood2024; 144 (14): 1521–1531