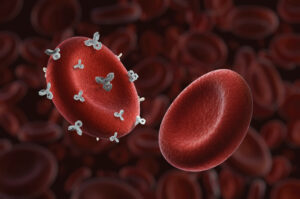
Of the approximately 400 RBC blood group antigens, only ABO/D are matched for routine transfusions. Some RBC blood group antigens are more immunogenic than others based on the number of patients transfused who develop alloantibodies. To better understand how amino acid substitutions affect the immunogenicity of blood group antigens, researchers used the AlphaFold2 artificial intelligence model in addition to multiple other programs to predict the 3-D structure of nine blood group antigens with amino acid substitutions: Kell blood group glycoprotein (K), basal cell adhesion molecule (Lua), urea transporter 1 (JKa), RhCE (E, c, C) glycophorin A (M), glycophorin B (S), and the atypical chemokine receptor 1 (Fya). Based on the number of patients who develop alloantibodies after transfusion or pregnancy, the four most immunogenic amino acid substitutions occurred in K, Jka, Lua, and E in what was predicted to be in β-strand, coils or helix regions, which are rigid, ordered regions with reduced accessibility. Lower immunogenetic amino acid substitutions in c, C, M, S, and Fya were predicted to be in unfolded terminal arms or surface accessible loops, but the confidence of these models was lower than for the highly immunogenic antigens. Results suggest that the more highly immunogenic amino acid substitutions may cause more structural disruption in ordered regions compared to more flexible or disordered regions. Future models that consider glycosylation and interactions with other membrane proteins will lead to more insight into the immunogenicity of amino acid substitutions in blood group antigens.
References:
- Howe JG, Stack G. Relationship between immunogenicity and protein structure at amino acid substitution sites of blood group antigens. Blood. 2025 Jul 24;146(4):504-517. PMID: 40163810.
- Walser P. Predicting blood group antigens: accessible or not? Blood. 2025 Jul 24;146(4):409-410. PMID: 40705389.