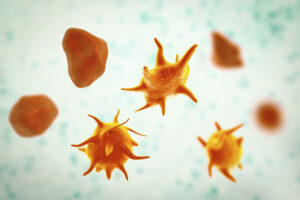
Approximately 2 million units of platelets are transfused each year in the United States, but there are many drawbacks and safety concerns with donor-derived platelets, including bacterial contamination and a short shelf life. In addition, 5% to 15% of patients develop alloimmune platelet transfusion refractoriness (allo-PTR) to human platelet antigens, such as HLA antibodies. In the first human clinical trial, researchers in Japan transfused autologous engineered platelets into a 55-year old woman with aplastic anemia with allo-PTR. Without a compatible platelet donor, researchers generated induced pluripotent (iP) stem cells from the patient’s own peripheral blood mononuclear cells. Immortalized mega-karyocyte progenitor cells (imMKCL) were then generated from the iP stem cells. After validation, these imMKCL were used to produce platelets (iPSC-PLTs) in a bioreactor with a cocktail of drugs to promote platelet proliferation, maturation, and preservation of function. These engineered platelets were then transfused back into the patient in escalating doses over several months. The transfusions were well tolerated, and the patient did not experience severe side effects over the one-year of follow-up. In addition to more human clinical trials, the cost and production time of engineering autologous platelets must be overcome before they are routinely used for transfusions.
References: