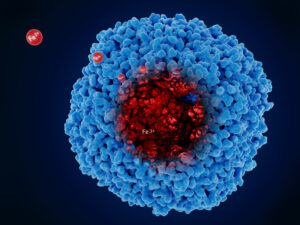
With each whole blood donation, donors lose approximately 250 mg of iron and have a higher risk of developing iron deficiency (ferritin <15 µg/L) and low hemoglobin levels. Blood collection centers primarily focus on hemoglobin levels to prevent iron deficiency and anemia in donors. Due to recent research showing that ferritin-guided donation intervals reduce iron deficiency, many centers are now monitoring donors’ iron stores and recommending iron supplementation. Questions remain, however, about gastrointestinal discomfort, donor return rate, and optimal iron formulations and dosages. To address some of these questions, researchers in the Netherlands randomized repeat whole blood donors with low ferritin (15 to 30 µg/L; n=830; 56% female) to receive either 0 mg (placebo), 30 mg or 60 mg ferrous bisglycinate (a highly absorbable iron formulation with fewer digestive side effects than traditional iron supplements) either daily or on alternate days. After 56 days of iron supplementation, only 1% of donors taking 60 mg daily were iron deficient compared with 4% of those taking 60 mg on alternate days, 10% and 7% of those taking 30 mg daily and on alternate days, respectively and 51% and 49% of those taking placebo daily and on alternate days, respectively. Daily supplementation with 60 mg of iron was also the most effective regimen for preventing low ferritin and low hemoglobin levels. Furthermore, gastrointestinal discomfort was low in all study arms and not significantly different. While iron supplementation is safe and effective for repeat donors and protects against iron deficiency, further research is needed for first-time donors and the intention of all donors to return while taking iron supplements.
Reference: