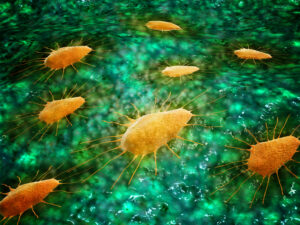
Transfusion-related acute lung injury (TRALI) is a rare, life-threatening adverse transfusion reaction that is difficult to predict and treat. The pathophysiology of TRALI is complex and not well understood. TRALI is dependent on both the inflammatory state of the transfusion recipient and other anti-leukocyte/endothelial-reactive antibodies delivered via a blood transfusion. Conflicting results on the role of the complement system have been reported, but recipient macrophages and polymorphonuclear neutrophils (PMNs) are essential for antibody-mediated TRALI pathology. To better understand the role of complement in TRALI induction, researchers used a mouse model based on the anti-MHC class I murine TRALI-inducing antibody 34-1-2S. Murine TRALI was complement driven and Fc- and C5- dependent but did not require FcɣR binding in mice. Furthermore, 34-1-2S antibody-mediated TRALI was associated with increased macrophage trafficking from the lungs to the blood compared to control mice. In addition, C5a acted as a chemoattractant for PMNs in the lungs of mice with antibody-mediated TRALI, and increased neutrophile extracellular traps (NETS, net-like structures formed from decondensed chromatin and antimicrobial peptides and enzymes extruded from neutrophiles) were observed. In humans, complement activation markers (IL-6, IL-8, C-reactive protein, and C5a) and NET marker levels were higher in the plasma levels of confirmed TRALI cases (n=53) compared to healthy controls (n=30). Results suggest that targeting the complement system and particularly C5, may be a promising therapeutic target for treating patients with antibody-mediated TRALI.
Reference: